Last month, The News-Gazette published an article on how the increased presence of fentanyl is leading to more opioid overdose deaths locally and beyond. Between Christmas Eve and Christmas Day 2021, there were four suspected overdose deaths in Champaign-Urbana. All four deaths were men between the ages of 27 and 30, three of them in the same house, and one who was about to begin a drug court self-help program. The article notes statistics from the Illinois Department of Public Health that reveal in Illinois, opioid deaths have increased from 1,072 in 2013 to 2,944 in 2020. A look at the opioid dashboard for Champaign County indicates a general upward trend in overdoses, both fatal and non-fatal, and points to a demographic that is mostly white, male, and within the 25-34 age group.
It’s difficult to remember that we have other public health crises happening, when our worlds are still so dominated by COVID and with a secondary epidemic of gun violence constantly hanging over our community. It’s important to know the extent of this issue locally, what resources are available, and what can work to address the problem. It’s an issue that, like gun violence, is an overwhelming one that requires complex solutions. We can’t arrest and prosecute our way out of it without looking at underlying causes.
In 2018, the New York Times asked 30 panelists to hypothetically spend $100 billion to solve the opioid crisis — this was a few months after the Trump administration declared it a public health emergency, but had yet to reveal any specific plans. Their answers fell into four general categories: treatment, harm reduction, decreasing demand, and decreasing supply. An aggregate chart revealed that 47% of that money should go towards treatment, 27% to address demand, 15% for harm reduction, and 11% to restrict supply. We took a look at what is happening here in Champaign County, related to these solutions.
Treatment
Champaign-Urbana Public Health District website has a page that lists affordable treatment centers in Champaign County, with a list of services and types of insurance accepted at each facility, but it’s focused on adolescents. Cunningham Township has a section with addiction resources on their community resources page. C-U at Home has a list of substance abuse clinics and detox centers. It didn’t seem that any one website had a full listing of options. Here are the main options for treatment in Champaign County:
-
Carle Addiction Recovery Center: Provides a range of services from inpatient detox to counseling and intensive outpatient and medically assisted treatment. Patients who show up in the emergency department due to overdose or drug related issues are referred here.
-
Rosencrance: Part of a large network across Illinois, they offer detox, residential and outpatient treatment, as well as recovery centers and sober homes for post treatment transition.
-
Prevention and Treatment Services (P.A.T.S.): Offers substance abuse assessments, groups and counseling.
-
The Pavilion: Their New Choice Center for Addiction Recovery is a 28-day inpatient program for detoxification and addiction treatment.
-
Safe House: Part of the Canaan Development Foundation; their men’s and women’s programs are 12 month residential programs with a religious component.
-
Champaign Treatment Center: An outpatient facility with counseling and methadone treatment.
Reducing Demand
These are solutions that are preventative in nature, and are very similar to those we might see in gun violence prevention, like community development and post-incarceration support. In the New York Times article, Dr. Anna Lembke, the medical director of addiction medicine at Stanford, said: “Until we provide people with an alternative source of dopamine, in the form of family connections, meaningful work and a sense of purpose in their lives, the problem of addiction will continue to grow.”
Mayo Clinic provides a list of common risk factors for opioid misuse, and the first three are poverty, unemployment, and family history of substance abuse. Though it’s difficult to pinpoint organizations in our community that are specifically targeting those who are at highest risk for opioid addiction, those particular risk factors highlight the importance of the work of Cunningham Township, C-U Public Health, the Housing Authority of Champaign County, United Way, First Followers, C-U Trauma and Resilience, and so many more.
Drug Court is specifically meant to “develop substance-free, productive citizens and break the cycle of criminal recidivism.” Individuals who are facing drug charges enter an intensive program with a team consisting of the State’s Attorney, Public Defender, Court Services, Rosencrance, the Judiciary, the Sheriff’s Department, Family Services, Champaign Treatment Center, and Safe House. The website states that three in four graduates do not commit a crime within four years after, though only one in three people who are sentenced to drug court graduate.
Harm Reduction
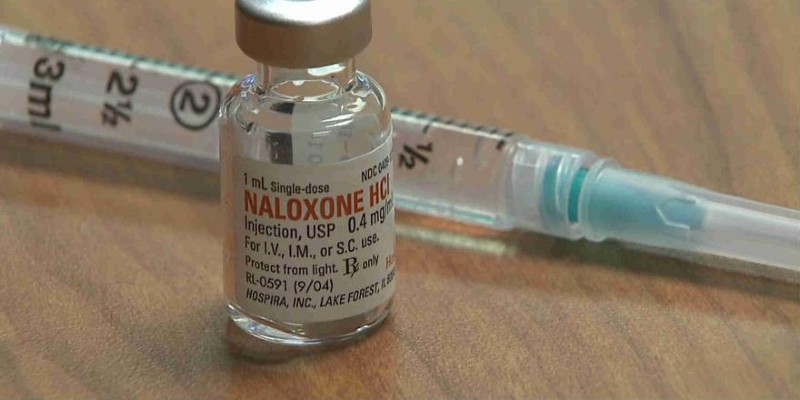
This strategy focuses on making drug use safer, rather than trying to keep people from using. A big part of this is increasing the availability of naloxone, or NARCAN, as a way to save someone from an overdose. C-U Public Health offers free NARCAN and training on how to use it to anyone 18 and older. You can do this during business hours on a walk-in basis. There’s been a recent push for library employees to be trained, something that’s recently been implemented in Chicago.
C-U Public Health also provides syringe exchange, in an effort to reduce the spread of HIV and hepatitis through needle sharing.
Reducing Supply
A small number of experts placed this at a high level of importance, and it includes both local federal law enforcement related to the proliferation of drugs into communities, but it also relates to monitoring opioid prescriptions through an electronic database and secure prescription drug drop boxes. The latter was recently discontinued at our local police departments due to safety concerns. All states, including Illinois, have a Prescription Monitoring Program. The research is fuzzy on whether it makes a huge difference in terms of reducing opioid misuse.
After examining the resources available, we’re wondering what others think of how we deal with opioid addiction in our community. Are we doing enough? What can be done to keep the problem from escalating further? Do the organizations serving those suffering from addiction need more from our local, state, and federal governments?
The Editorial Board is Jessica Hammie, Julie McClure, Patrick Singer, and Mara Thacker