 Last month marked the 38th anniversary of Roe v. Wade, and we ran an article highlighting three different women’s abortion stories. In an open call for anyone’s experience with reproductive health access, I came across two very unique personal stories, both from could-be abortion providers. With fewer and fewer abortion providers practicing in the United States (87% of all U.S. counties lack one), I was extremely interested in the delicate decisions that go into determining one’s future in medical practice. I was surprised to find how difficult it is to even receive training to be an abortion provider, and am concerned that future providers might be frightened away from the abortion side of reproductive health due to our tense and even lethal political climate. These two stories will be broken into two separate articles. Today, we meet Dr. G.H.
Last month marked the 38th anniversary of Roe v. Wade, and we ran an article highlighting three different women’s abortion stories. In an open call for anyone’s experience with reproductive health access, I came across two very unique personal stories, both from could-be abortion providers. With fewer and fewer abortion providers practicing in the United States (87% of all U.S. counties lack one), I was extremely interested in the delicate decisions that go into determining one’s future in medical practice. I was surprised to find how difficult it is to even receive training to be an abortion provider, and am concerned that future providers might be frightened away from the abortion side of reproductive health due to our tense and even lethal political climate. These two stories will be broken into two separate articles. Today, we meet Dr. G.H.
SP: What kind of political/religious background were you raised in, if any?
GH: I was raised in a fairly conservative and religious household. My parents taught Sunday school in our church; my father is a Republican, and my mother always shaped her opinions to align with his. I always got the impression they operated under a “don’t ask, don’t tell” policy when it came to controversial topics like homosexuality or abortion. It wasn’t until I was an adult and brought up these topics that I realized my parents viewed such actions as “morally wrong.”
SP: When did you first become interested in medicine? Why?
GH: I was born with a congenital anomaly that required me to undergo intensive operations when I was four years old. As a result of the trust and admiration that I developed during my frequent interactions with the medical community, I decided to pursue medicine and give back to the field.
SP: Where are you in your academic/career path? Please explain for us non-med folks out there.
GH: I am currently in my final year of medical school. I have applied for residency positions and am awaiting the results of the match, a process by which applicants are paired to hospitals across the country. I have applied to programs throughout the Midwest. 
SP: How did you become interested in reproductive health?
GH: OB/GYN is a required six-week clerkship at my academic institution. Every third-year medical student spent three weeks in the department of gynecology, and three weeks in obstetrics. There is time spent in the OR, clinic, and the Labor and Delivery unit. Prior to this experience, I had spent a summer volunteering at our local women’s health clinic.
SP: Did you provide, or witness abortion procedures?
GH: I did not witness any elective abortion procedures at my academic institution. These types of procedures are not allowed in the hospital where I am training. This hospital performs D&Cs for spontaneous abortions (aka, miscarriages), but if a woman wishes to terminate her pregnancy, she is referred to a women’s health clinic. During my volunteer experience at such a clinic, I witnessed a great number of abortion procedures, both medical and surgical. Our institution’s chapter of Medical Students for Choice also organized a procedures day, where we were taught how to perform a surgical abortion on a papaya.
SP: How were you educated about these procedures at school and on-the-job?
GH: The topic of abortion was discussed only briefly during the first and second didactic years of my medical education. We were not instructed on how to perform these procedures in a classroom. I observed a D&C during my OB/GYN rotation for a spontaneous abortion.
SP: What was your initial reaction to these procedures?
GH: I was actually fascinated by the procedure. From a surgical standpoint, it was appealing because it is quick, requires a thorough understanding of the female anatomy, and it taught me a lot about fetal development. I was surprised by its simplicity and minimal invasiveness.
SP: Current political and religious discourse is tense regarding abortion, but the climate in the medical community seems to be overlooked unless something extreme occurs, like Dr. Tiller’s murder. What was it like during your time providing abortions? Will you choose to provide abortions long-term?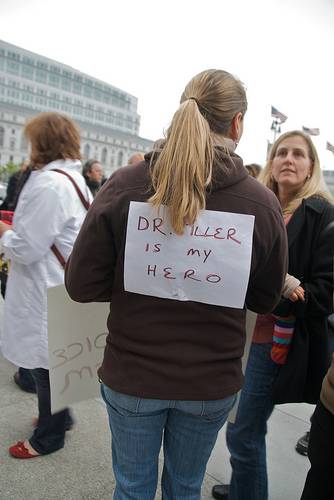
GH: I am now training in a part of the country where abortion is viewed in a very negative light. In fact, I am training in the very state where Dr. Tiller was murdered. There are very few abortion providers in our state, and in fact, sometimes women have to drive 400-500 miles to obtain the services they need. To deter this, protesters have placed anti-abortion billboards all along the major highways of our state. When I worked at the women’s health clinic, there were daily picketers and people making threatening comments. As a board member for our chapter of Medical Students for Choice, I would receive hurtful emails in response to our broadcast advertisements for speakers or luncheons we organized. We had poor turnout to our fundraisers and lectures. I continue to feel, especially since the death of Dr. Tiller, that this state is a particularly hostile environment toward abortion providers, and in keeping the safety of my own family in the forefront, have decided to not continue to provide abortions long-term.
SP: Would you consider providing abortions if you became employed in a less choice-negative state?
GH: When I am finished training, I will be board-eligible in pediatrics, adult and child neurology. I have heard of and met some pediatricians who provide abortions simply to help meet the demand. I have thought a lot about whether I’d be willing to provide that service, and I feel that it would be, if I were seeing general pediatrics patients in my practice. However, after three years of training in neurology and given the even greater need, if imaginable, for child neurologists in our state, I foresee my clinic patient population consisting of solely neurological diagnoses.
SP: You sound like you are very comfortable talking about abortion and taking time to understand the complexities of why the service needs to be available to women. How do you perceive colleagues’ reactions to the topic?
GH: I felt many of my medical school colleagues and faculty members distance from me when they heard about my interest in providing abortions. I have had colleagues say some pretty hurtful things after I have shared some of my thoughts on the topic or discussed the highlights about conferences I have been to, etc. Some of the comments include things like, “Wow, I never would have pictured you as someone being so immoral,” or “I’m disappointed in you,” and “How can you sleep at night??” Thankfully, those responses are not the norm. My closest friends in medical school have been supportive. They let me know from time to time that they don’t agree with my perspective, but they are very receptive to my thoughts on contraception and preventing pregnancy.
 SP: On that note, what role/responsibility do you think medical providers have to talk with women about pregnancy options?
SP: On that note, what role/responsibility do you think medical providers have to talk with women about pregnancy options?
GH: It is definitely the responsibility of the medical provider to explain all the options available to a woman when she faces a pregnancy for which she was not prepared, and I feel that they are required to deliver that information free of bias. I do not feel that any provider should be obligated to perform a service or procedure with which s/he does not feel comfortable, even if that includes writing a prescription, but all providers should be obligated to provide information on all the options a woman has before her, and refer her to other clinics where those services can be obtained. I perceive that it is easier for patients to discuss their feelings and thoughts with [a female] than it might be with a male provider. But, to be quite honest, I think it’s safe to say that when a woman has made the decision to terminate her pregnancy, she just wants anyone, regardless of gender, to listen to her and help her through the process.
SP: Under what circumstances should a woman NOT get an abortion (assuming she is not being coerced into the decision)?
GH: I cannot think of a circumstance in which a woman should be forced to carry out a pregnancy if she does not want to. It does not matter if she is financially stable or in a loving, caring relationship or has excellent supports. If continuing the pregnancy would cause her physical, mental, emotional or spiritual harm, then she should be free to act as she chooses.
SP: Did providing/witnessing abortions change any personal political/religious/moral beliefs for you?
GH: Surprisingly, given the environment in which I was raised, I have always considered myself a person with liberal opinions, and have supported women who chose to have an abortion. My experience only reaffirmed why it is so important to educate people like myself to continue to make these services available to women.
SP: What role should the medical community play in decreasing the number of abortions, if any?
GH: I’m so glad you have targeted the root of this issue: No one is pro-abortion. No one wants women to have abortions. The goal is to prevent unwanted pregnancies in the first place. The medical community should have discussions with young women and men regarding safe sex practices and contraception at an early age. It’s interesting that pregnancy is often considered a risk associated with having sex, as opposed to a likely outcome. Young people should be educated that pregnancy is the outcome of unprotected sex in 30% of cases, and that if they are not prepared to deal with the responsibility associated with that outcome, they need to do something to preemptively reduce the likelihood of pregnancy occurring.
SP: Are you partnered? Did your time in ob/gyn spark any interesting or new discussions with your significant other?
GH: I am married, and we have a 14 month old son. I completed my volunteer experience at a women’s clinic before I was pregnant, and would come home daily to talk about my thoughts regarding abortion with my husband. His outlook on abortion is the same as mine, so it was nice to share my interest and enthusiasm with him. While I started my OB/GYN rotation, we had an 8 week old infant at home to take care of, so our conversations rarely had anything to do with what either of us had done at work that day, but we did have many discussions regarding the behavior of my academic institution.
SP: Do you think differently about abortion procedures now that you’re a mother?
GH: Before I was pregnant, I will admit, I could appreciate what women feel when they discover they are pregnant, but I certainly could not empathize with them. I didn’t understand at that time what an immense responsibility it is to carry out a pregnancy and to become a mother. I think that now I have even more respect for women who choose abortion.
SP: What impacted you the most during your time providing abortions?
GH: I was deeply conflicted by trying to balance the gratitude and appreciation I received from the women and their families who benefited from our services with the hateful comments I would hear walking into work or the gruesome posters I would pass on my way across campus. I understood the need for more abortion providers, but I also understood what a great risk that would be for myself and my family [to continue to practice]. I saw family practitioners and even pediatricians being trained to perform these procedures, simply to increase the number of providers in our state. That provider desperation struck me the most.
SP: What are your hopes and fears regarding access to abortion in your state and the U.S. as a whole?
GH: I fear that if services are not more easily accessible in our state that women may pursue avenues to terminate their pregnancies that are unsafe and unhealthy. I worry for the women who finally get the courage to tell their OB/GYN or family practitioner that they are pregnant and that they want to terminate the pregnancy and are stigmatized and shunned from the clinic. My heart breaks for the woman 350 miles away from the nearest abortion provider who has to face an anti-abortion billboard every 25 miles en route. Most of all, I fear for the brave providers in our state who have courageously continued to provide to this highly underserved population. My hope is far-fetched: I hope that one day medical providers will feel as comfortable providing an abortion as they would performing an appendectomy or a tonsillectomy; that women could obtain services within a 25 mile radius of their home; that [abortion] training would be offered to all medical students as part of the standard curriculum.
——
Stay tuned for Part 2, a male potential provider’s look at abortion access and training in Illinois.








